-Multiple sclerosis is a chronic inflammatory neurological disease which is generally diagnosed between 20-40 years
-Effects range from mild to severe
-There is no known single cause of MS, but many genetic and environmental factors have been shown to contribute to its development
Pathophysiology:
-Auto-immune disorder affecting the central nervous system.
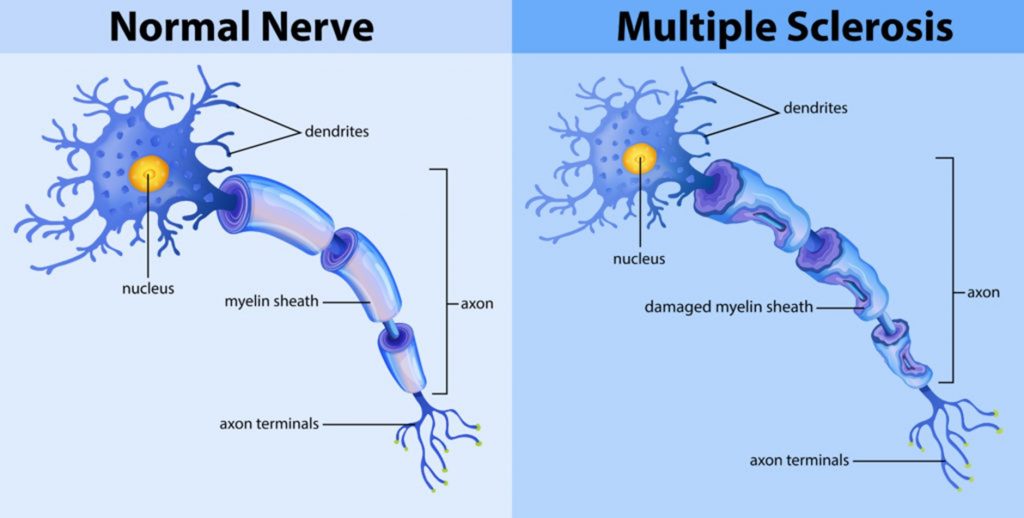
-The myelin sheaths of nerves are attacked and degraded.
-These sheaths protect the axons and provide insulation to facilitate nerve conduction.
-In MS, the body’s own immune system mistakenly attacks and damages the fatty material called myelin which surrounds the nerves. Myelin is important for protecting and insulating nerves so that the electrical messages that the brain sends to the rest of the body, travel quickly and efficiently.
-As the myelin breaks down during a MS attack – a process called demyelination – patches of nerves become exposed and then scarred, which render the nerves unable to communicate messages properly and at risk of subsequent degeneration. This means that the brain cannot talk to other parts of the body, resulting in a range of symptoms that can include a loss of motor function (e.g. walking and hand and arm function, loss of sensation, pain, vision changes and changes to thinking and memory).
In short:
-Damage to the myelin sheath -> Nerve impulses lost or not properly conducted ->Neural signals lost or altered
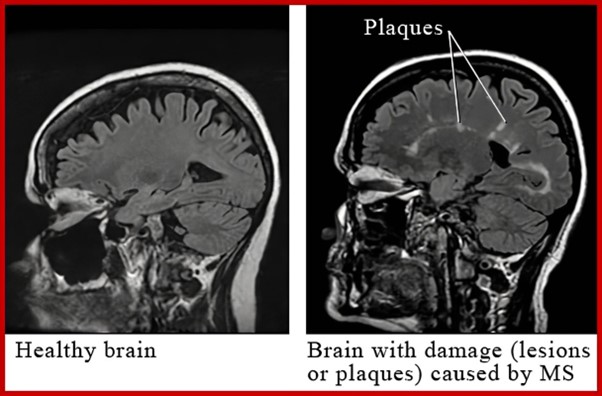
-Damage to the myelin sheath -> Hardened, sclerosed plaques within white and grey matter
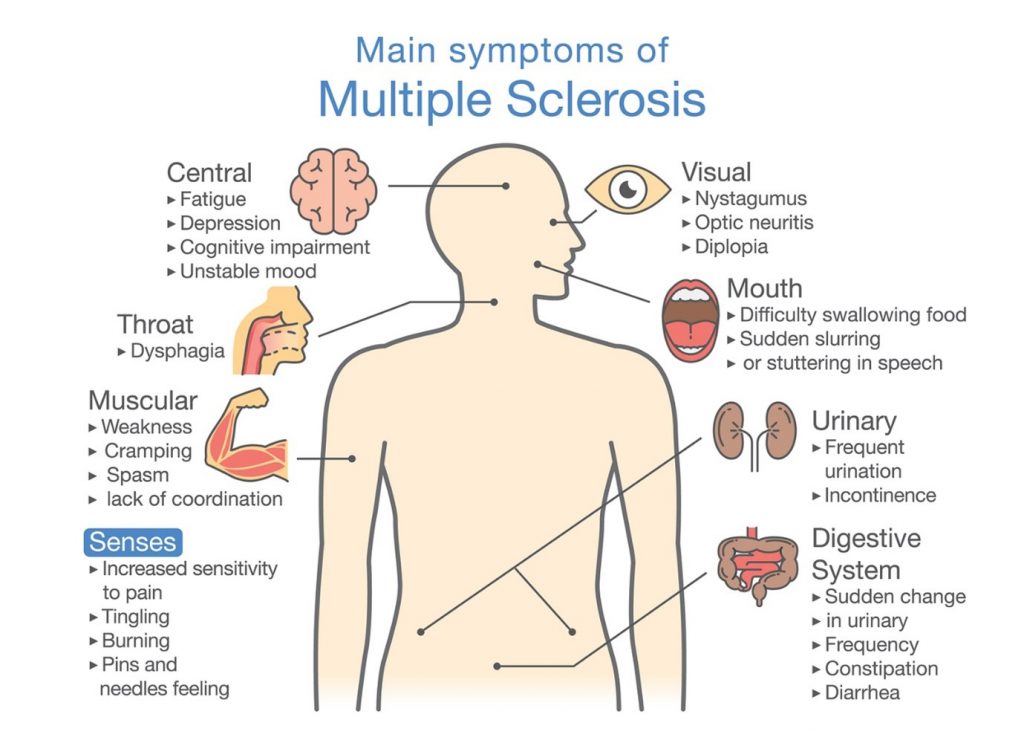
Symptoms
-Decreased gait and balance
-Weakness and fatigue
-Spasticity
-Changes in sensation
-Visual disturbances
-Cognitive and emotional impairments
-Sleep disruption
-Loss of bladder and bowel control
-Depression and decreased functional ability
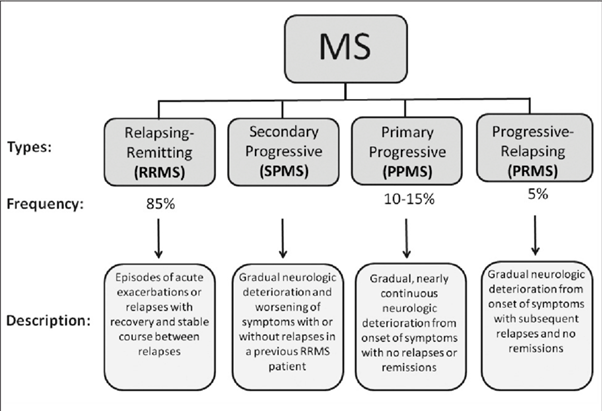
Characterised by the pattern of relapses and remissions
1. Relapsing-remitting
Comes and goes but does not deteriorate
2. Primary progressive
No remission, with gradual deterioration
3. Secondary progressive
Starts as relapsing-remitting, but becomes progressive
4. Progressive relapsing
Progresses steadily, with intermittent severe episodes
Diagnosis:
Need a number of confirmatory tests and excluding other possible conditions.
-MRI to detect plaques
-Analysis of cerebral spinal fluid for monoclonal antibodies
Key requirements for diagnosis:
-Two clinical attacks
-Affecting separate areas of the central nervous system
-Attacks occurring at two different times
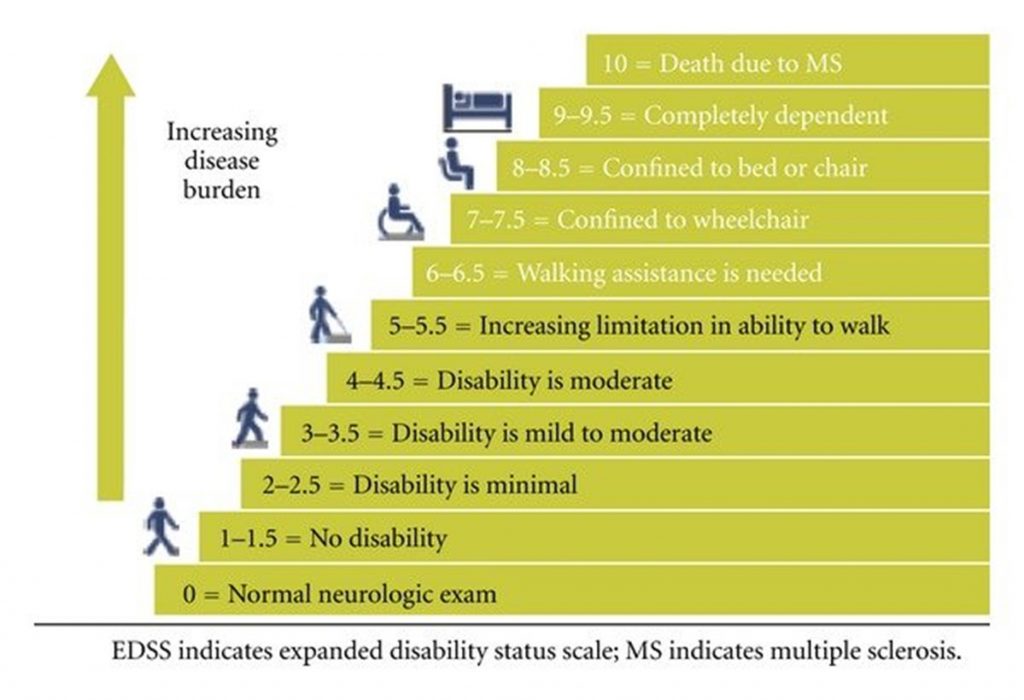
Severity
-Classified using clinical features
-Functional Systems Score or Kurtzke Expanded Disability Status Scale (EDSS).
-EDSS most widely used and accepted measure of severity
-Scores range from 0 – normal neurological exam, to
-5: ambulatory without aid for about 200m, disability impairs ADL, to
-9.5: Unable to communicate effectively or eat or swallow, to
-10: death
-Disease progression is complex and varies between individuals.
Diagram used for classification of disability, the Expanded Disability Status Scale (EDSS)
Management
Assistive devices:
- Canes, walkers and crutches
- Orthotics
- Functional electric stimulation
- Wheelchairs and motorised scooters
- Cooling vests
ACSM’s Exercise Management for Persons with Chronic Diseases and Disabilities, 4E
Effects on exercise response
-Tend to be inactive
-Low levels of cardiovascular and muscular fitness Fatigue one of the main barriers to physical activity Those with multiple sclerosis experience heat sensitivity.
-Exercise response might include:
-Low or very low level of functioning
-Dyspnea on exertion
-Exaggerated pressor and chronotropic responses weakness and fatigues easily
-Low thermal stress tolerance
Effects of Exercise
-Regular exercise can increase peak VO2 Increase muscle strength
-Increase range of motion
-Note! Might see a temporary worsening of symptoms when starting an exercise program, together with an increase in fatigue.
-These symptoms usually goes away 30min after exercise session Insufficient research to provide evidence for most beneficial exercise program and effects of exercise on impairments.
Exercise testing: guidelines-
-Follow CDD4 recommendations
-Submaximal testing is preferred.
-Do not perform any maximal tests.
-Assessments could be adversely affects by medication, secondary conditions and disease severity.
-Include assessments for: Balance, sensation and flexibility.
-Time of day (later in day) and heat / higher temperatures could adversely affect performance during the exercise assessment.
Guidelines for exercise prescription
Supervised exercise:
-Tailor exercise program according to person’s needs and abilities Ensure that exercises are performed safely and properly
-Offer counselling support and to help overcome anxiety and fear related to exercise.
Goal:
-Maintain functional ability and independence
-Prevent boredom and monotony, so offer a variety of exercises and programs. Group activities provide opportunities for socialisation
-Reduce the risk of developing co-morbidities such as osteoporosis, hypertension and diabetes.
-When starting an exercise program, begin at a low level and use familiar activities.
-Gradually increase as tolerated.
-Focus on increased adherence
-If needed, provide alternative exercises and focus on fun.
-Multiple short bouts throughout the day, with different levels of intensity and duration.
-Encourage patients to ‘listen to their bodies’ and to let this guide their participation.
Aerobic training:
Mode
-Large muscle groups
-Easily accessible activities like walking
-Hydrotherapy, especially for those with muscular skeletal problems Other activities the client enjoys – cycling, gardening
Frequency
-4-5 days per week
Duration
-Start with what can be tolerated.
-Aim for 40 minutes per session
-Could be 20 minutes, if including resistance training
Intensity
-Self-selected pace or walking speed
-Use talk test as a measure of intensity Gradually increase until RPE = 3 to 5 out of 10
Progression
-Gradually increase from self-selected walking pace to 40 minutes of walking over a 4 week period.
-Increase intensity as tolerated.
-Consult with primary care giver before embarking on high intensity exercise.
Resistance Training:
Mode
-Functional gravity-based exercises
-Weight training can be performed in those who are interested and motivated
Frequency
-2 – 3 days per week
Duration
-Body weight exercises – one set during TV commercials (30s) Weight training: 1 set of 8-12 reps to fatigue
Intensity
-Sit to stand: 8 reps
-Alternative: stair steps X 10 steps Arm curls: 8 reps with 4kg weight 50-70% of 1RM
Progression
-Build up gradually doing as many sets as can be tolerated
-Arm curls and weight training – increase to 2 sets over 8 weeks
Flexibility training:
Mode:
-Hips, knees, shoulders, and neck
Frequency:
-3 days per week
Duration:
-20s-30s per stretch
Intensity:
-Maintain stretch below discomfort point
Progression:
-Discomfort point should occur at ROM that does not cause instability
-Varies from person to person from joint to joint



