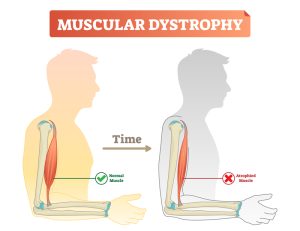
Muscular dystrophy is the broad term for a group of genetic diseases which cause progressive weakness and wasting of muscles. Many genes help to develop proteins which make and protect muscles and each variation of muscular dystrophy can be caused due to altercations to a specific gene which relate directly to muscular function.
Types of Muscular Dystrophy
There are over 30 types of muscular dystrophy, with the most common types being:
Duchenne Muscular Dystrophy (DMD): Condition affects males and females aged 2-5 which causes altercations to a protein in muscles called dystrophin that helps keep cells intact. DMD first affects the proximal muscles of the body however spreads to the distal segments of the body. It has been found that the lower limbs are affected before the upper body and results in difficulties balancing, walking/ running, and jumping. Other symptoms of DMD includes enlarged calf muscles, waddling gait, hunched posture, and tight muscles. DMD also influences both cardiac muscles and pulmonary functions.
Becker Muscular Dystrophy (BMD): Affects males and females ages 6-30 (more common in 13-20) which is caused by dystrophin being influenced and being produced too short. It is characterised by the degeneration/ wasting of the muscles as well as affecting cardiac muscles. The signs and symptoms of BMD also includes decreased cognitive ability, motor delay, gastrointestinal affects, decrease respiratory function. Walking altercations/ impacts usually occur around 15-16 years. In BMD, the if the muscle calls are damaged and repaired, it is replaced by fat and scar tissue instead of muscle cells. BMD usually affects muscles of the hips, pelvis, thighs, and shoulders. BMD is a progressive condition and increases in severity as age increases.
Myotonic Dystrophy: the age of onset of MD is typically within adulthood and is characterised by prolonged muscular contractions (myotonia), inability to relax post-muscular contraction, slurred speech, locking of the jaw. This disease can also influence the electrical signal of the heartbeat and increases the risk of developing diabetes. There are two types of MD, type 1 MD affects more distal segments of the body where type 2 affects more proximal segments of the body.
Facioscapulohumeral Dystrophy (FSHD): a rare genetic disease that affects the muscles in a child’s face, shoulders, upper arms, and lower/ distal legs. The age of onset it typically before 20years and weakness spreads to other areas of the body. Children with FSHD are unable to walk a result of this disease. Common symptoms of FSHD include scapular winging, inability to reach overhead, difficulty pursing lips, difficulty initiating full smile, eyes not closing fully during sleep, and weakness in the ankle or pelvic muscles that make it more difficult to walk.
Limb-Girdle Muscular Dystrophy (LGMD): group of diseases that cause weakness and wasting of the muscles proximal to the torso of the body including shoulders, proximal arms, pelvic region, back, core, and quadriceps/ hamstrings. This disease causes complications to spinal alignment (scoliosis, lordosis, kyphosis), winging of the shoulder blades, stiffness or looseness in the joints, minimal contraction of posterior lower limb muscles, and excessive growth of the calf muscles. No intelligence or cognitive impacts are seen in LGMD.
Congenital Muscular Dystrophies (CMD): a group of muscular dystrophies which are apparent at or near birth. CMD result in joint stiffness or looseness which may also influence spinal alignment, intellectual disability, eye defects, seizures. Infants with CMD may be slow to meet or never meet motor milestones such as rolling over, sitting, walking. The types of CMD can impact severity, symptoms, and rate of progression of the disease.
Exercise for Muscular Dystrophy and Considerations for Exercise
Exercise can benefit individuals with muscular dystrophy if the appropriate load, volume, and intensity is applied to receive the best benefits possible. Exercise can have numerous psychological and physiological positive effects for the general population, such as improvements in self-estimate and plasma endorphin concentrations, increased strength, endurance, function, quality of life, decrease cardiovascular complications, decrease loss of cognitive function, and improve mental health. Research currently demonstrates that partaking in resistance-based exercise can minimise and counter the muscle loss/ atrophy that occurs with muscular dystrophy.
Because of muscle degeneration in muscular dystrophy, there may be the risk of exercise-induced adverse effects such as overwork weakness following supramaximal, high- intensity exercise. Each type of muscular dystrophy results in weakness in specific areas and thus exercise must be tailored towards the individual. Individuals with muscular dystrophy also fatigue a lot quicker compared to the healthy population, take longer to recover from a session, and take a longer period to see results. A wholistic view should be applied when developing an exercise program including aerobic components, resistance-based exercise for lower and upper limbs, core and posterior strengthening, and balancing exercises.
For aerobic exercises, start with short bouts of low-moderate intensity and ensure that the exercise is completed with comfort and minimal pain. This can be through walking, cycling, swimming/ hydro, e.c.t. Ensure to include rest periods when needed and gradually/ slowly increase the length per bout when ready. Aerobic exercise should be completed 3-4x per week and ensuring some rest days in between or worked around resistance-based exercise days.
For resistance-based exercises, this should include body weight exercises, small free weights, and light bands to begin with. Testing and knowledge of the condition should be applied for resistance-based exercises as different areas of the body will be more impacted by the condition and thus the volume/ load that area requires will be different as well as the possible range of motion. Major muscle groups should be utilised within the upper limbs, lower limbs, and core/ back. Some excessive eccentric or muscle lengthening exercises should be avoided when first complete strength training and only incorporate concentric based exercises to minimise muscle fatigue, muscle damage, increase muscular power, and allow for gradual progression or intensity. Strength/ resistance-based exercises should be completed at least x2 per week and allowing for 1-2 days rest in between allowing for the muscles to recover. The intensity of the exercises should be low-moderate and comprise of 4-6 exercises per session whilst applying the FIIT principle. Considerations should be to minimise unsafe positions of the muscles/ joints/ ligaments of the body as well as being cautious of neck, back, and posture.
Stretching should also be incorporated into the training regime to ensure that muscle fatigue is being minimised whilst also encouraging more range of motion within the body. Take care not to over stretch weak muscles or joints that are already very mobile and should be primarily focused on the major muscle groups and muscles that are tight. Intensity of the hold should be a comfortable intensity and able to be held for 30-40s for 1-2 rounds.