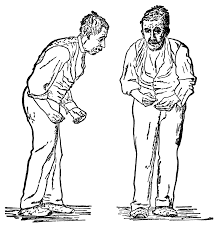
Physical activity, together with its ameliorative effects on Parkinson’s disease (PD) symptoms, remains a relatively unappreciated factor which may be beneficial for the treatment outcome. Contemporary evidence supports the positive effects of non-pharmacological approaches to PD symptom management, in particular the effects of the exercise on both, motor and non-motor symptoms.
Exercise is an essential impulse for various cells (e.g.myocytes) to upregulate the expression of insulin-like growth factor type 1 (IGF-1), brain neurons to increase production of neurotrophic factors such as brain derived neurotrophic factor (BDNF) and limiting for neuroinflammation. Moreover, exercise regulates plasticity in the hippocampus and the cortex, CA1 and entorhinal cortex, and increases fine discrimination. The effect of PA, especially on the nervous system, results in increased molecular adaptations in neuronal function. However, many of the mechanisms by which exercise exerts its effects in the brain remain largely unknown.
People with Parkinson’s disease often do not do much exercise which is associated with a loss of fitness. This can worsen the effects of the disease and any other conditions they may have. For example, heart disease, muscle weakness, osteoporosis (weak bones), trouble sleeping, constipation and depression can all grow worse. Loss of fitness also increases the risk of falls, especially in people with Parkinson’s disease, who are already much more likely to fall than healthy people. This tendency to fall and consequent injury (e.g. hip fractures) can eventually result in loss of independence and early admission to nursing homes.
Resistance training increases strength in older people and people with Parkinson’s disease. Recent research indicates that high resistance progressive exercise is effective with initial levels of 30-40% 1RM being increased to 70% 1RM and from 1 to 3 sets of 8 repetitions. 1 RM is the maximum amount of weight one can lift in a single repetition for a given exercise. However, the best program for these exercises has yet to be determined. It is also important to be mindful that people with Parkinson’s disease tire easily, and that it may be best to use an individually tailored approach that accounts for these limitations.
Treadmill walking is frequently used for people with Parkinson’s disease. You can either walk slowly or use a training program that gradually increases your walking speed. Although the optimal program has yet to be determined recent research indicates that longer duration low intensity walking is more effective than high intensity short duration walking. If you have difficulty walking, body weight supports can be used. Even if you have trouble walking or ‘freeze’ when trying to move, you may still be able to cycle. Stationary cycling is ideal if you have this problem. Pacing yourself or deliberately increasing the cycling rate can improve your heart and lung function and your walking ability. It also “exercises” other neural circuits important for movement other than those involved in locomotion. ‘Cueing exercises’ involve walking while listening or seeing cues that mimic the rhythm of walking. These exercises can help improve your walking movements and overcome difficulty with gait initiation and freezing. ‘Dance’ provides exercise to music that can facilitate functional and expressive movement. It also provides important social interaction and can lead to improvements in perceived quality of life. In ‘dual tasking’ exercises, you do a secondary task (e.g. forming words or counting backwards) while walking. These exercises usually try to improve one aspect of walking at a time (e.g. step length). Dual tasking is very proficient in challenging balance as well, for example balance on the spot or functional balancing and stating names of countries or animals.