What is Peripheral Artery Disease?
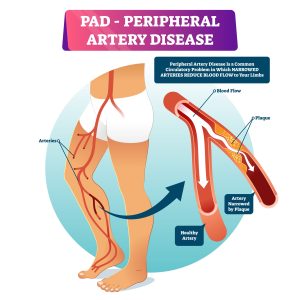
Peripheral artery disease (PAD) is caused by atherosclerotic narrowing of the arteries supplying the lower limbs. The most classic symptom of PAD is intermittent claudication, which is ischaemic muscle pain that usually presents in the calves (but can include the thighs or buttocks) and is precipitated by exertion and relieved with rest. It is believed that the pain is due to a mismatch between the oxygen demand and an inadequate blood supply (due to the narrowed arterial pathway).
It is estimated that >200 million people have PAD worldwide, with symptoms ranging from none to severe. Patients with PAD have a higher burden of cardiovascular disease and are at greater risk of major cardiovascular events. Another major issue is the severe decline in functional capacity which are comparable to patients with patients with heart failure and reduced ejection fraction. The reduction in functional capacity is commonly caused by a decline in walking capacity, which may be up to less than <50% of healthy aged, matched controls. This also impacts a patient’s mental health, which reduces quality of life and further avoidance of physical activity, which leads to worsening of functional ability and elevated mortality.
The prevalence of PAD rises with age and affects a substantial proportion of the elderly population (>20% in >80year old individual). Other factors that increase PAD risk include a history of smoking, diabetes, age, and dyslipidaemia.
Treatment for patients with intermittent claudication involves secondary prevention of cardiovascular disease risk which includes;
- Smoking cessation
- Diet changes
- Lipid modification
- Statin therapy
- Antiplatelet therapy
- Management of diabetes and hypertension
However, the primary treatment to address the functional impairments outline above is for patient so to engage in supervised exercise training.
Benefits of Exercise Training:
Currently there is high quality evidence showing that supervised exercise programs elicit important improvements in both pain-free and maximum walking distance compared with no-exercise control in people with IC. Aerobic exercises has shown to elicit cardiovascular adaptations such as increased blood flow, changes in microcirculation, endothelial function and oxidative metabolism – which all assist to reduce symptoms and pain. Other improvements in exercise include improved walking distance and functional capacity, along with improved quality of life and mental health, and most importantly, reducing the risk of developing serious cardiovascular conditions. Guidelines on how people with PAD can exercise are shown below.
Exercise Guidelines:
- Aerobic Exercise: Structured Walking is the modality of exercise with the strongest evidence and is recommended in several national and international guidelines. This involves walking on a treadmill or track walking at an intensity that elicits moderate to maximal claudication pain. Alternate forms of exercises such as upper and lower body cycling can be used. All patients should aim to accumulate at least 30 mins of aerobic activity, at least 3x a week for at least 3 months, ideally in the form of walking exercise to near max claudication pain.
- Intensity: 4-5 on claudication pain scale.
- Treadmill protocol: following warm up, walk at a speed and grade that induces claudication pain within 3-5 min. Stop walking and rest when claudication pain reaches a moderate to strong level. When the pain has abated, resume walking until the moderate-strong pain recurs. Repeat for at least 30mins. In subsequent exercise bouts, the speed or grade of walking is increased if you can walk for >10 min without reaching moderate claudication pain. Can start at lower pain levels as tolerate but should be encouraged to increase the intensity of pain achieved as a progression too.
- Upper and lower limb ergometer: 10 sets of 2 mins if upper and lower ergo conducted twice a week for at least 3 months. Moderate intensity of 13-14 on a Borg RPE scale.
- Resistance exercise:yet to be included as the sole therapy for PAD treatment, recommended to be done with aerobic exercise. Moderate to high intensity (14-16 on Borg scale), 6-8 exercises (e.g. leg press, knee flexion, knee extension, chest press, seated row) targeting major muscle groups of the upper and lower body, 2-4 set of 10-15 reps,2-3 sessions per week.
For the best outcomes, it is strongly recommended to complete these exercises with an accredited health professional, as they can complete functional assessments and ensure these exercises are done safely, at a level that is tolerable, and can provide progressions over time.